PHC Department of Anesthesiology
The PHC Department of Anesthesiology is dedicated to providing high quality, safe and patient centered care for patients within Providence Health and the community at large. The Department consists of over 60 Anesthesiologists who contribute clinical expertise and innovation, cutting-edge research, and leadership in Providence perioperative services. PHC Anesthesiologists work at St. Paul’s Hospital and Mount St. Joseph’s Hospital.

The Department of Anesthesiology consists of specialists in:
Cardiac Anesthesiology & Perioperative Echocardiography
Acute and Chronic Pain Medicine
The PHC Department of Anesthesiology also has an active Research and Quality Improvement Program spanning the different subspecialties.
Department Leadership
Acute and Chronic Pain Medicine

Overview
St. Paul’s Hospital Pain services provides pain management through a interdisciplinary approach to patients in both in-patient and out-patient areas. The team consists of Occupational Therapists, Physcial Therapists, Nutritionists, and Physician from Anesthesiology, Family Practice, Internal Medicine, Psychiatry, Neurosurgery and Rehabilitation Medicine

Our Pain Medicine Practice Includes:
- Medical management of chronic & complex pain conditions including Complex regional pain syndrome
- Interventional pain procedures under Ultrasound & fluoroscopy
- Neurostimulation for Chronic pain and Targeted drug delivery for Oncology pain

Fellowship Opportunities
Learn more about Fellowship opportunities or contact us at anesthesia.fellowships@ubc.ca
Leadership

Cardiac Anesthesiology & Perioperative Echocardiography
Overview
The Heart Center at St. Paul’s Hospital is the provincial referral centre for highly complex cardiac care, including heart transplantation and mechanical circulatory support, adult congenital procedures, laser lead extractions, and septal myectomies.
Cardiac Surgery Intensive Care Unit (CSICU)
St. Paul’s Hospital’s Cardiac Anesthesiologists are experts in managing these patients through extensive experience in the cardiac operating rooms, transesophageal echocardiography, and the cardiac surgical intensive care unit (CSICU).
In 2021, we performed:
- Over 1000 open-heart surgeries,
- 250 transcatheter valve implants,
- 60 lead extractions,
- 40 extracorporeal membrane oxygenation (ECMO) initiations,
- 20-25 heart transplants,
- 15-20 Ventricular assist device (VAD) implantations,
- 5 Thoracic endovascular aortic repairs (TEVAR).
Fellowship Opportunities
Learn more about Fellowship opportunities or contact us at anesthesia.fellowships@ubc.ca
Currently Recruiting Research Studies
Bilateral paravertebral blockade for improvement of quality of recovery following cardiac surgery(P-QOR): A randomized controlled trial PI: Dr. Terri Sun
The efficacy of pecto-intercostal fascial plane catheters for reduction of sternal pain in cardiac surgery patients with complete median sternotomy: A randomized, placebo-controlled trial PI: Dr. Ron Ree and Dr. Tim Ting Han Jen
CODEX Trial: Cognitive outcomes after Dexmedetomidine sedation in cardiac surgery patients PI: Dr. Raja Rajamohan
Leadership
Perioperative Medicine

Overview
Perioperative medicine is a collaborative, evidence-based practice that has emerged as a subspecialty within Anesthesiology. The perioperative medicine pathway begins at the moment that the patient and physician(s) decide on surgery and ends when the patient makes a full recovery and returns to baseline function. The goal is to ensure optimal patient outcomes by identifying (risk stratification) and communicating risks to the surgical patient before the surgery, making recommendations about anesthetic management during the surgery and potentially increasing monitoring after the surgery. It is most applicable to high-risk patients undergoing major surgery, and it considers the implications of the stress of a major surgery on long-term diseases such as diabetes or chronic kidney disease.
Benefits of having a Perioperative Medicine system in place
- Before surgery: optimizes treatment of chronic diseases & determines risk of proposed surgery, discussion of risks in the context of patient goals and expectations
- During surgery: can improve patient outcomes without treating the actual index disease (E.g., optimal pain control intra-operatively may increase the chances of a speedy recovery)
- Early after surgery: patients will end up at the correct level of care based on their individual need, potential ongoing surveillance by a perioperative medicine specialist while in the hospital
- Later after surgery: acts as a bridge between the hospital and primary care. Helps coordinate follow-up appointments for complications, changes in home medications, or family medicine specialist/NP notifications
Learn more about St. Paul's Hospital Perioperative Medicine
Currently Recruiting Research Studies
Fellowship Opportunities
Learn more about Fellowship opportunities or contact us at anesthesia.fellowships@ubc.ca
Leadership

Regional Anesthesiology

Overview
The Regional Anesthesia Division is a group of dedicated, innovative, and enthusiastic practitioners. We strive to be leaders in providing clinically excellent care for our patients. We perform approximately 3500 regional anesthesia techniques per year. As well, our site is the primary regional anesthesiology teaching center for the UBC Anesthesiology residency program, and we have a flourishing sub-specialty fellowship program that continues to mentor physicians from across Canada and around the world. We have an innovative research program where we are seeking out novel methods to provide safe, effective anesthesia and pain relief for our surgical patients. We provide education and coaching to practicing physicians through local, national, and international lectures and workshops. We have also recently been involved with at-the-bedside remote-mentorship in regional anesthesia techniques to our colleagues throughout rural British Columbia.

SPH Block Room
St. Paul’s Hospital features a busy block room associated with the main operating rooms which is staffed daily with a dedicated Regional Anesthesiologist and an Anesthesia Assistant. We provide single-shot and continuous peripheral nerve blocks, as well as thoracic epidurals for anywhere from 10-15 surgical patients per day. We also provide a home-catheter service for select patients so they can recover more comfortably after being discharged from the hospital. We have an active hip-fracture regional anesthesia pathway established to provide optimal pain relief for some of our frailest patients.
SPH Surgical Procedure Room (SPR)
In addition, St. Paul’s also operates a separate high-volume outpatient perioperative program where extremity surgeries are performed solely using regional anesthesia techniques in a swing-room model. One Surgeon, one Regional Anesthesiologist, and two operating rooms allow for minimal waiting between cases, along with efficient discharge of patients who are ready to eat, drink, and head home very quickly after their surgery.
MSJ Block Room
At Mount St. Joseph’s Hospital we have established a block room program dedicated to providing regional anesthesia for breast cancer surgery. Patients can choose to avoid a general anesthetic and have improved pain relief after their surgery. We were recently awarded a Best Patient Safety & Quality Award for the introduction of this program to Providence Health Care
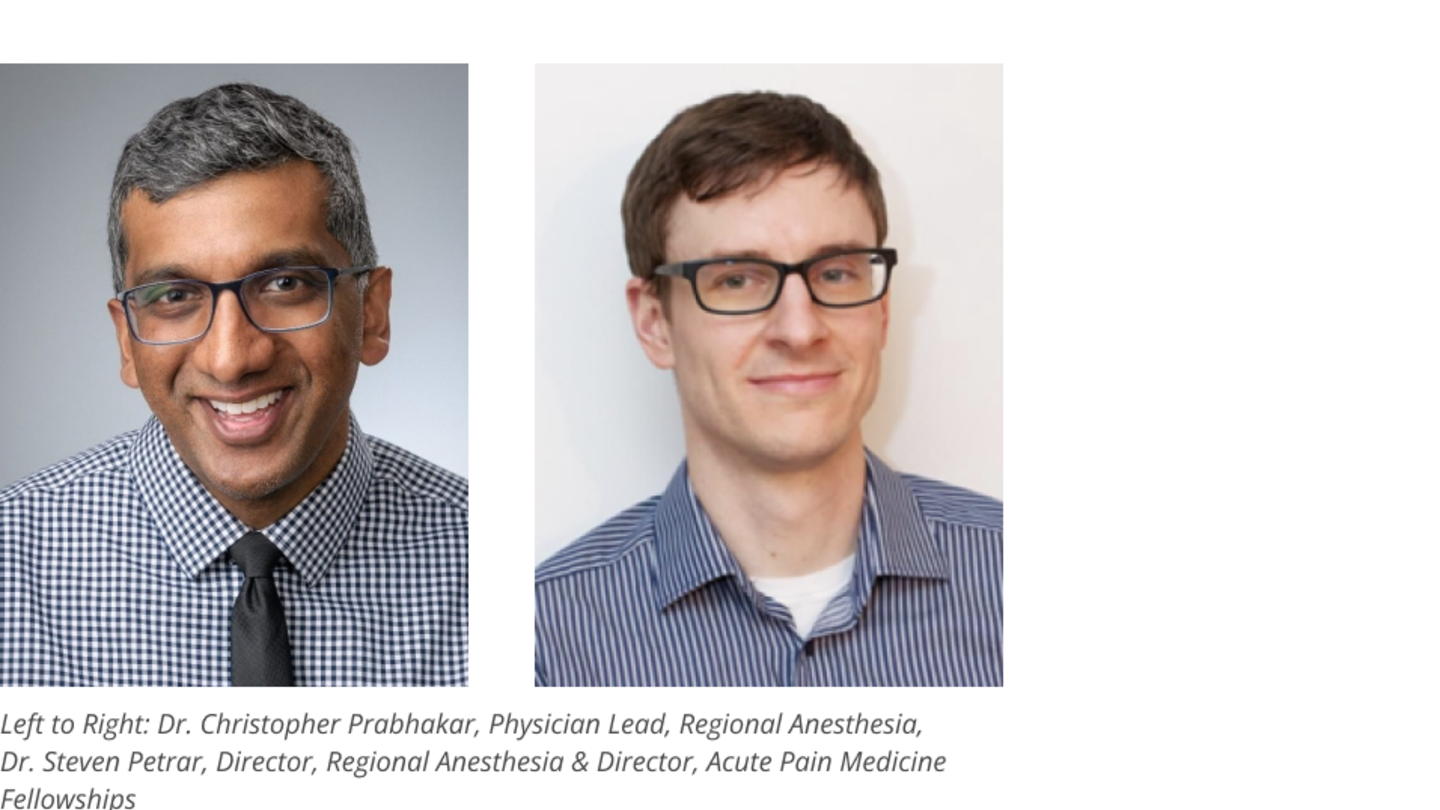
Leadership
Fellowship Opportunities
Learn more about Fellowship opportunities or contact us at anesthesia.fellowships@ubc.ca
Currently Recruiting Research Studies
Bilateral paravertebral blockade for improvement of quality of recovery following cardiac surgery(P-QOR): A randomized controlled trial PI: Dr. Terri Sun
The efficacy of pecto-intercostal fascial plane catheters for reduction of sternal pain in cardiac surgery patients with complete median sternotomy: A randomized, placebo-controlled trial PI: Dr. Ron Ree and Dr. Tim Ting Han Jen
CODEX Trial: Cognitive outcomes after Dexmedetomidine sedation in cardiac surgery patients PI: Dr. Raja Rajamohan
Research and Quality Improvement

Overview
The PHC Department of Anesthesiology has an active and vibrant Research Program. From Investigator-led RCTs to Quality Improvement Initiatives and participation in multi-site trials, our clinician researchers are passionate about conducting rigorous patient-centred research. Approximately 20 of our Anesthesiologists are Principal or Co-Investigators on active research projects. Our Research Program centres around the following research themes: Perioperative Medicine, including Brain Health and Patient Centred Outcomes, Regional Anesthesia, Acute and Chronic Pain Medicine and Cardiac Anesthesiology.

Leadership

Dr. Flexman’s research is focused on neuroanesthesia, including perioperative stroke and brain health. After finishing anesthesia residency at UBC, she completed a fellowship in neuroanesthesia at the University of California San Francisco and specializes in the effects of anesthesia and surgery on the brain. Dr. Flexman also serves as president-elect for the Society for Neuroscience in Anesthesiology and Critical Care (SNACC), and the past-chair of the Neuroanesthesia Section of the Canadian Anesthesiologists’ Society.

Dr. Chau is an Obstetric Anesthesiologist and Physician-Scientist with joint appointments at St. Paul’s and BC Women's Hospitals. Following his Anesthesiology Residency at UBC, he pursued a combined Clinical and Research Fellowship in Obstetric Anesthesiology at Brigham and Women’s Hospital under the mentorship of Dr. Lawrence Tsen, MD, completed the UBC Clinician Investigator Program and obtained a Masters of Medical Sciences degree in Clinical and Translational Research at Harvard Medical School. Dr. Chau conducts clinical and translational investigations with a focus on the impact of anesthesia on maternal and fetal outcomes. His research interests include neuraxial analgesia and anesthesia techniques, obstetric general anesthesia, peri-delivery optimization and patient safety.

Dr. Montemurro is an anesthesiologist specializing in regional anesthesia. Dr. Montemurro has advanced training in Quality Improvement, and is an active participant in the Physician-led Quality Improvement Initiative, the past safety chair of the BC Anesthesiologists’ Society, and a member of the Provincial Surgical Executive Committee (PSEC). Her most recent QI projects include improving the perioperative administration of sub-cutaneous heparin, creating a multi-disciplinary hip fracture surgery optimization program, and implementation of cognitive aids in anesthesiology.

Nicola has a background in Health Sciences and a Masters in Health Administration. She oversees and guides the Anesthesia research program at St. Paul's Hospital. Nicola facilitates collaboration between clinician researchers, institutions and industry sponsors. She manages research finance and supervises multiple Research Coordinators and Research Assistants.